Opioids are a prescription drug class most commonly prescribed for the treatment of moderate to severe pain. They include drugs such as oxycodone, hydrocodone, morphine, and fentanyl. Improper use of these medications, however, can lead to an overdose which can be a life-threatening medical emergency.
According to the Substance Abuse and Mental Health Services Administration (SAMSHA), administering naloxone (Narcan) in a timely manner after a suspected overdose can help prevent opioid-overdose related deaths. Naloxone is an opioid antagonist that reverses the effects of the opioids and can reverse the respiratory depression caused by an overdose.
As applicable to the care setting and individual, resuscitation efforts should take into consideration the individuals’ overall care plan, including advanced directives.
Step 1: Check for signs of an opioid overdose
- Unconsciousness or inability to awaken.
- Small or pinpoint pupils.
- Troubled breathing, slow or shallow breathing (respiratory rate < 6/minute).
- Fingernails or lips turning blue/purple or pale skin.
- Faint heartbeat.
- Limp arms and legs and / or inability to speak.
If an opioid overdose is suspected, alert Medical and attempt to arouse the individual:
- If not responding to verbal cues, attempt physical stimuli such as a sternum rub or rubbing upper lip to arouse individual.
- If the person responds, assess whether he or she can maintain responsiveness and breathing.
- Continue to monitor the person, including breathing and alertness, and try to keep the person awake and alert.
If the individual does not respond, proceed to call 911, provide rescue breathing if appropriate, and administer 1 dose of naloxone.
Step 2: Activate Emergency Medical Services (EMS) Pathway / Call 911 for Help
- If no emergency medical services (EMS) or other trained personnel is on the scene, activate the 911 emergency system immediately.
- Follow the dispatcher’s instructions.
Step 3: Administer naloxone
Follow the administration guide below for the dosage form of naloxone you have available.
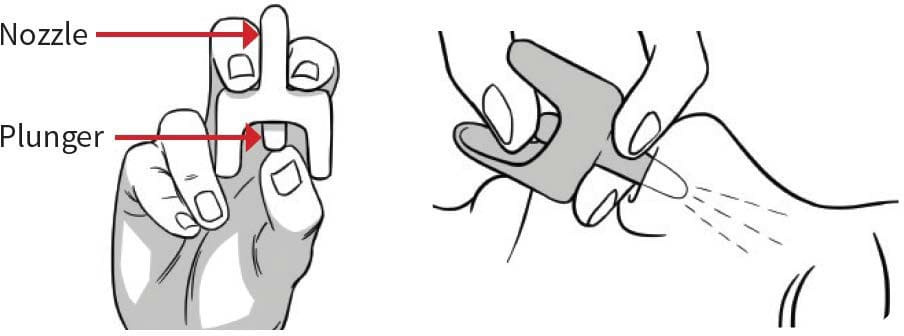
How to administer naloxone nasal spray:
- Peel back the package to remove the device.
- Hold the device with your thumb on the bottom of the plunger and 2 fingers on the nozzle.
- DO NOT test or attempt to prime the nasal spray, it contains a single dose of naloxone.
- Place and hold the tip of the nozzle in either nostril until your fingers touch the bottom of the individual’s nose.
- Press the plunger firmly to release the dose into the nose.
- Repeat with a second dose to the other nostril if there is no response after 2-3 minutes.
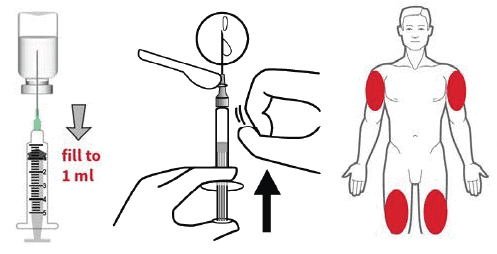
How to inject naloxone intramuscularly:
- Inspect the naloxone solution for discoloration or particles. Discard solution if not it is not clear.
- If using a vial: Uncap vial and remove syringe from its packaging. Insert the needle into the rubber membrane on the naloxone vial, turn the vial upside down, drawn up 1 mL and withdraw the needle.
- If using a prefilled syringe: Remove the protective cap from the syringe, attach the provided needle and remove the cap.
- With the needle pointing up, gently tap the syringe to remove visible bubbles and push excess air from the syringe prior to administration.
- Insert the needle into the muscle of the upper arm or thigh, through clothing if necessary, and push on the plunger to inject all the naloxone.
- Repeat with a second dose if there is no response after 2-3 minutes.
Note: Administering naloxone may induce opioid withdrawal-like symptoms including anxiety, chills, muscle aches, high blood pressure and heartrate, fever, nausea, vomiting and diarrhea. These symptoms are not life-threatening and should subside in about 2 hours. Do not give naloxone to an individual with a known allergy to naloxone or any of its components. Naloxone is not likely to produce harm or clinical effect when given to individuals that are not opioid intoxicated or opioid dependent, if overdose agent is in doubt.
** Repeat dosing may be indicated for potent opiate agonists (i.e., fentanyl), reversing large opiate quantities or for long-acting opiates due to shorter half-life of naloxone in comparison, and provided under medical direction and authorization.
Step 4: Support the Person’s Breathing and Airway
- If you are capable, continue rescue breathing or CPR on the individual until spontaneous breathing is restored or support is deemed no longer medically necessary. Supporting respiration is a critical intervention for opioid overdose and may be life-saving on its own.
Step 5: Monitor the Individual’s Response and Provide Supportive Care
- Individuals should be monitored for recurrence of signs and symptoms of opioid toxicity for at least 4 hours from the last dose of naloxone. In cases where an individual overdosed on long-acting opioids, monitoring should continue for a longer period of time until they are cleared by a medical provider.
- Continue to support the individual until EMS or other medical support arrives and takes over. The individual should be transferred to the emergency department as quickly as possible, even if the naloxone successfully restored breathing and they are responsive.
References:
- SAMHSA. “Opioid Overdose Prevention Toolkit.” Jun. 2018, https://store.samhsa.gov/product/Opioid-Overdose-Prevention-Toolkit/SMA18-4742 Accessed 21 Nov. 2022.
- NIDA. “Naloxone DrugFacts.” National Institute on Drug Abuse, 11 Jan. 2022, https://nida.nih.gov/publications/drugfacts/naloxone Accessed 21
Nov. 2022.