The 2023 GOLD Report: Global Strategy for Prevention, Diagnosis, and Management of Chronic Obstructive Lung Disease
On an annual basis the Global Initiative for Chronic Obstructive Pulmonary Disease (GOLD) releases a strategy report covering all of the previous year’s major research articles and details updates to existing therapeutic recommendations for the prevention, diagnosis, and management of the condition. The 2023 release is a thorough overhaul, citing 387 new references, including several major longitudinal COPD studies published over the last few years.
GOLD 2023 Highlights to the Update [1,2]:
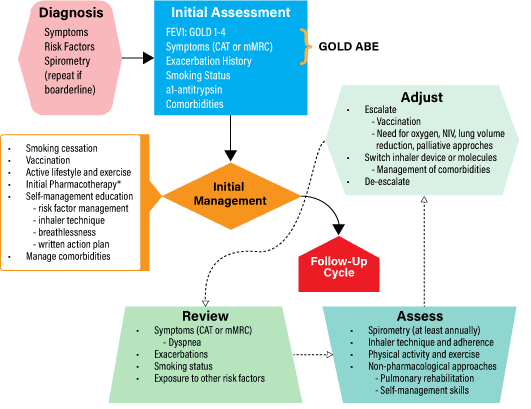
Classification and Treatment Initiation
- Revision of initial pharmacotherapy treatment algorithm based on redefined classification of patients with COPD
- Updated grading considerations for disease exacerbation
COPD Management Cycle [1]:
GOLD 2023 Redefined COPD [1,3]
- New taxonomy for COPD is added to classify etiology and describe the condition
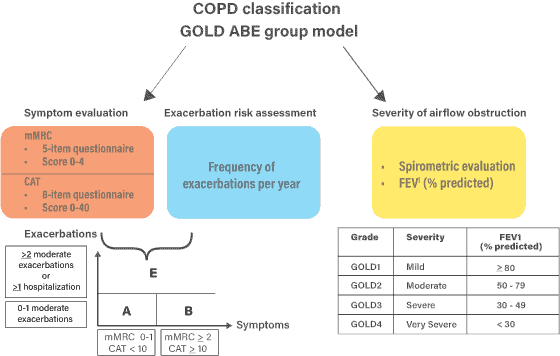
New ABE Assessment Tool and Treatment Recommendations
- Change to the COPD assessment tool is meant to better recognize and address the clinical relevance of exacerbations, independent of the level of baseline symptoms.
- Retained: ‘A’ → less symptomatic, low-exacerbation-risk
- Retained: ‘B’ → more symptomatic, low-exacerbation-risk
- Removed: ‘C’ → less symptomatic, high-exacerbation-risk
- Removed: ‘D’ → more symptomatic, high-exacerbation-risk
- Created: ‘E’ → Exacerbation-prone patients
| GOLD 2023 Initial Pharmacotherapy [1,2] | ||
|---|---|---|
| ≥ 2 moderate exacerbations OR ≥ 1 leading to hospitalization | Group E: LABA + LAMA* Consider LABA + LAMA + ICS* if blood eos ≥ 300 |
|
| 0 or 1 moderate exacerbations (not leading to hospitalization) | Group A: A bronchodilator | Group B: LABA + LAMA* |
| mMRC 0-1, CAT < 10 | mMRC ≥ 2, CAT ≥ 10 | |
*Single inhaler therapy may be more convenient and effective than multiple inhalers
See below section on exacerbations for updated classification algorithm; table refers to the number of
exacerbations experienced per year.
| Rescue short-acting bronchodilators should be prescribed to all patients for immediate symptom relief | |
|---|---|
| Group A | – All offered bronchodilator treatment (either a short- or a long-acting) based on its effect on breathlessness. — If available and affordable a long-acting bronchodilator is the preferred choice except in patients with very occasional breathlessness. – This should be continued if benefit is documented. |
| Group B | – Treatment should be initiated with a LABA + LAMA combination LABA + LAMA is superior to a LAMA monotherapy with regard to several endpoints. Combination therapy is recommended providing there are no issues regarding availability, cost and side-effects. — If LABA + LAMA is not considered appropriate → no evidence to recommend one class of long-acting bronchodilators over another (LABA or LAMA) for initial relief of symptoms in this group of patients. – In the individual patient, the choice should depend on the patient’s perception of symptom relief. |
| Group E | – LABA + LAMA combination was the highest ranked treatment group to reduce COPD exacerbations (versus monotherapy with long-acting bronchodilators) — LABA + LAMA is the preferred choice for initial therapy in group E patients providing there are no issues regarding availability, cost and side-effects. – Use of LABA + ICS in COPD is not encouraged → If there is an indication for an ICS, then LABA + LAMA + ICS has been shown to be superior to LABA + ICS and is therefore the preferred choice. |
Did You Know…There are new key points outlined for use of each medication class!
- Inhalation Devices
- Consider availability of the drug in the device; minimize number of different device types
- Switch should never occur without proper information, education, and medical follow-up
- Patient’s cognition, dexterity, and strength must be taken into account
- Bronchodilators
- LABAs and LAMAs are preferred over short-acting agents EXCEPT for patients with only occasional dyspnea, and for rescue in those on long-acting maintenance therapy. Combination therapy with LAMA+ LABA is preferred over monotherapy.
- LAMAs provide greater exacerbation and hospitalization risk reduction compared to LABAs and are a recommended component of therapy in those who have experienced multiple moderate or any severe exacerbations.
- SABA + SAMA combination therapy is more effective than either agent alone.
- Inhaled bronchodilators are recommended over oral therapy, i.e. theophylline.
- Anti-inflammatory Agents
- Long-term monotherapy with ICS is not recommended
- In patients with COPD and concomitant asthma, treatment should always contain an ICS
- Severe to very severe airflow limitation, chronic bronchitis, and exacerbations: consider addition of PDE4 inhibitor to regimen with long-acting bronchodilator with/without ICS
- Other Treatments
- Severe hereditary alpha-1 antitrypsin deficiency and established emphysema → consider as candidate for alpha-1 antitrypsin augmentation therapy
- Antitussives are not well supported and not recommended to manage COPD symptoms
- Drugs approved for primary pulmonary hypertension (i.e. vasodilators) are not recommended for patients with pulmonary hypertension secondary to COPD.
- Low-dose long-acting oral and parenteral opioids may be considered for treating dyspnea in COPD patients with severe disease
GOLD 2023 Exacerbations of COPD (ECOPD) [1]
- An exacerbation of COPD is defined as an event characterized by dyspnea and/or cough and sputum that worsen over < 14 days.
- The goals for treatment of COPD exacerbations are to minimize the negative impact of the current exacerbation and to reduce further exacerbation risk.
Key Points for Management of Exacerbations:
- Short-acting inhaled beta2-agonists, with or without short-acting anticholinergics are recommended as the initial bronchodilators to treat an acute exacerbation
- Systemic corticosteroids can improve lung function (FEV1), oxygenation, and shorten recovery time and hospitalization duration; duration normally no more than 5 days
- Antibiotics, when indicated, can shorten recovery time and hospitalization, and reduce the risk of early relapse or treatment failure; duration normally no more than 5 days
- Methylxanthines are NOT recommended due to increased side effect profiles
- Non-invasive mechanical ventilation should be first mode used in COPD patients with acute respiratory failure who have no absolute contraindication
| Intervention Class | Intervention | Patient Circumstances Compelling Use |
|---|---|---|
| Bronchodilators | LABAs LAMAs LABA + LAMA | – Exacerbation reduction and decrease of hospitalizations: — LABA + LAMA > LAMA > LABA – Monotherapy with persistent exacerbations → LABA + LAMA escalation |
| Corticosteroid Addition | Inhaled Corticosteroid (ICS) | – Higher blood eosinophil count indicates greater magnitude of success – Strongly favored in those with historical hospitalizations due to ECOPD – Necessary addition in those with concomitant asthma (or history of) – Consider if on dual bronchodilator regimen with persistent exacerbations – Consider withdrawal if pneumonia or serious side effects develop |
| Anti-inflammatory (non-steroid) | roflumilast (Daliresp) | – Consider in patients with FEV1 <50% predicted and chronic bronchitis, particularly if hospitalized for ECOPD within past year |
| Anti-infectives | Oral antibiotics, acute Long-term Macrolides Vaccination | – Consider short-course oral antibiotics with signs of bacterial infection – Long-term macrolide (azithromycin or erythromycin) therapy reduces incidence of exacerbations over one year — Avoid azithromycin with current smokers – Recommend proper vaccination to reduce risk of recurrence |
| Mucoregulators | N-acetylcysteine Carbocysteine Erdosteine | – In select populations (COPD patients not receiving ICS), regular treatment with agents reduces ECOPD risk and incidence – Erdosteine has significant beneficial effects on MILD exacerbations (regardless of concurrent treatment with ICS) |
Full information, management, and evidence can be found in the published 2023 GOLD Guidelines.
Citations:
- Agusti A, Celli BR, Criner GJ, et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease: 2023 Report. American Journal of Respiratory and Critical Care Medicine. 2022 Nov 14. Available from: https://goldcopd.org/2023-gold-report-2/
- Hess M. 2023 GOLD Report [Internet]. Irving (TX): American Association for Respiratory Care; 2023 Jan 19 [cited 2023 Mar 15]. Available from: https://www.aarc.org/an23-2023-gold-report/
- Czarnecka-Chrebelska KH, Mukherjee D, Maryanchik SV, Rudzinska-Radecka M. Biological and Genetic Mechanisms of COPD, Its Diagnosis, Treatment, and Relationship with Lung Cancer. Biomedicines. 2023; 11(2):448. https://doi.org/10.3390/biomedicines11020448