ADA Standards of Care in Diabetes Guidelines 2023 – What’s New?
Type 2 DM Pharmacotherapy Selection Update and Management Considerations for Older Adults:
Key updates related to T2DM pharmacotherapy from the 2023 ADA guideline include the following:
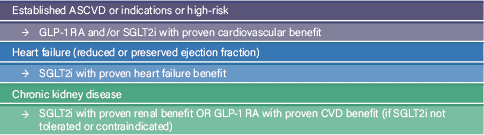
- Further emphasis for selecting pharmacotherapy (first-line and add-on therapies) based upon patient specific factors, comorbidities, and treatment goals (e.g., cardiorenal risk reduction in high-risk patients, glycemic and weight management, access, etc.).
- For T2DM patients at high-risk or established cardiovascular disease, heart failure and/or chronic kidney disease, glucose-lowering therapies with demonstrated cardiorenal benefit should be utilized where appropriate. These therapies are now recommended independent of the patient’s initial A1C% goal or metformin use.
| Drug Class | ASCVD | HF Effect | Renal Effect |
| GLP-1 RAs | Benefit: ■ dulaglutide ■ liraglutide ■ semaglutide (SUBQ) Neutral: ■ exenatide ER ■ lixisenatide ■ semaglutide (oral) | Neutral | Benefit: ■ dulaglutide ■ liraglutide ■ semaglutide (SQ) |
| SGLT2 inhibitors | Benefit: ■ canagliflozin ■ empagliflozin Neutral: ■ dapagliflozin ■ ertugliflozin | Benefit: ■ dapagliflozin ■ empagliflozin ■ canagliflozin ■ ertugliflozin | Benefit: ■ canagliflozin ■ dapagliflozin ■ empagliflozin Neutral: ■ ertugliflozin |
Drug therapies have been categorized by efficacy to help guide pharmacotherapy decision-making for patients with primary glycemic management or weight management goals.
| GLUCOSE LOWERING EFFICACY | WEIGHT LOSS EFFICACY | ||
| Category | Drug | Category | Drug |
| Very High | ■ Dulaglutide (high-dose) ■ Semaglutide ■ Tirzepatide ■ Insulin ■ Combination oral therapy ■ Combination injectable therapy (GLP-1 RA/insulin) | Very High | ■ Semaglutide ■ Tirzepatide |
| High | ■ GLP-1 RA (not listed above) ■ Metformin ■ SGLT2 inhibitor ■ Sulfonylurea ■ TZD | High | ■ Dulaglutide ■ Liraglutide |
| Intermediate | ■ DPP-4 Inhibitor | Intermediate | ■ GLP-1RA (not listed above) ■ SGLT2 inhibitor |
| Neutral | ■ DPP-4 Inhibitor ■ Metformin |
First approved dual GIP/ GLP-1 receptor agonist tirzepatide (Mounjaro®) added to guidelines
- Stimulates incretin effect, promoting insulin secretion and glucose clearance after meals
- Rated very high efficacy for A1C% and weight reduction
- Cardiorenal benefit currently under investigation
- Subcutaneous injection administered once weekly
- Gastrointestinal adverse effects may occur initially and decrease over time
See Section 9. Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes—2023 for
additional information, including recommendations for intensifying TIIDM therapy when indicated, using insulin and combination injectable therapy in this population. Link
Diabetes Care Considerations – Older Adults
Diabetes is a highly prevalent health condition in the aging population. Over one-quarter of people over the age of 65 years have diabetes, and one-half of older adults have prediabetes, with prevalence expected to increase over the coming decades.
To determine therapeutic approaches and targets for diabetes management, patient characteristics, functional status, comorbidities and overall care plan will need to be considered. The following table adapted from the ADA Guidelines provides a framework for considering treatment goals in older adults with diabetes.
| Patient characteristics/health status | Rationale | Reasonable A1C goal‡ | Blood Pressure Target |
| Healthy (few coexisting chronic illnesses, intact cognitive and functional status). | Longer remaining life expectancy. | <7.0–7.5% (53–58 mmol/mol) | < 130/80 mmHg |
| Complex/intermediate (multiple coexisting chronic illnesses* or two or more instrumental ADL impairments or mild-to-moderate cognitive impairment). | Intermediate remaining life expectancy, high treatment burden, hypoglycemia vulnerability, fall risk. | <8.0% (64 mmol/mol) | < 130/80 mmHg |
| Very complex/poor health (LTC or end-stage chronic illnesses** or moderate-to-severe cognitive impairment or two or more ADL impairments). | Limited remaining life expectancy makes benefit uncertain. | Avoid reliance on A1C; glucose control decisions should be based on avoiding hypoglycemia and symptomatic hyperglycemia. | < 140/90 mmHg |
Pharmacotherapy Considerations – Older Adults
Special care is required in prescribing and monitoring pharmacologic therapies in older adults.
Overtreatment of diabetes is common in older adults and should be avoided. In older adults with TIIDM at an increased risk for hypoglycemia, medication classes with low risk of hypoglycemia are preferred.
Insulin and sulfonylureas (i.e., glipizide) are considered high risk for hypoglycemia in older adults and should be considered for deprescribing where appropriate.
Deintensification of treatment goals is recommended to reduce the risk of hypoglycemia if it can be achieved within the individualized A1C target. Deintensification/ deprescribing refers to decreasing the dose or frequency of administration of a treatment or discontinuing a treatment altogether.
Example: If mealtime insulin < 10 units/ dose
- consider discontinuation of mealtime insulin, adjust basal or non-insulin therapy
Similarly, simplification of complex treatment plans (especially insulin) is recommended to reduce the risk of hypoglycemia and polypharmacy and decrease the burden of the disease if it can be achieved within the individualized A1C target. Treatment regimen simplification refers to changing strategy to decrease the complexity of a medication regimen, which may include:
- consolidating or changing administration times
- decreasing blood glucose checks
- decreasing the need for calculations, such as sliding scale
Each drug class used for TIIDM management in the older adult
| Metformin | First-line agent for older adults with T2DM. Contraindicated in those with advanced renal insufficiency and should be used with caution in those with impaired hepatic function or heart failure because of the increased risk of lactic acidosis. Monitor for B12 deficiency with long-term use. |
| DPP-4 Inhibitors | Generally well tolerated, with few side effects and minimal risk of hypoglycemia. |
| Medications: | Sitagliptin (Januvia), Saxagliptin (Onglyza) , alogliptin (Nesina), & linagliptin (Tradjenta) |
| Insulin Therapy | Once-daily basal insulin injection therapy is associated with minimal side effects is considered a reasonable option in many older adults. Multiple daily injections of insulin may increase risk for administration errors and hypoglycemia. Simplification of insulin regimens is recommended to reduce risk of adverse effects in older adults. |
| GLP-1 Receptor Agonists | In a systematic review and meta-analysis of GLP-1 receptor agonist trials, these agents have been found to reduce major adverse cardiovascular events, cardiovascular deaths, stroke, and myocardial infarction to the same degree for people over and under 65 years of age. Due to gastrointestinal side effects, drug class may not be appropriate for older adults experiencing unexplained weight loss or at risk for dehydration. |
| Medications: | dulaglutide (Trulicity), liraglutide (Victoza), semaglutide (Ozempic), exenatide (Byetta), & lixisenatide (Adlyxin) |
| Sodium-Glucose Cotransporter 2 Inhibitors | Analysis of CVOTs indicate that older adults have similar or greater benefits than younger people for those with established ASCVD, heart failure and chronic kidney disease. Side effects such as volume depletion, urinary tract infections and worsening urinary incontinence may limit use for in older adults. |
| Medications: | canagliflozin (Invokana), empagliflozin (Jardiance), dapagliflozin (Farxiga), & ertugliflozin (Steglatro) |
| Insulin Secretagogues | Sulfonylureas and other insulin secretagogues are associated with hypoglycemia and should be used with caution. If used, sulfonylureas with a shorter duration of action, such as glipizide, are preferred. Glyburide and glimepiride are on the Beers List due to their longer half-life and risk for prolonged hypoglycemia. |
| Thiazolidinediones | Use cautiously in older adults on insulin as well as those with or at risk for heart failure (fluid retention), osteoporosis, falls or fractures, and/or macular edema. |
| Medications: | pioglitazone (Actos) |
See Section 13. Older Adults: Standards of Care in Diabetes—2023 for additional information, including screening recommendations for geriatric syndromes and neurocognitive functions, managing hypoglycemia risk in older adults, supporting algorithms and tables for simplification of treatment regimens and deprescribing in older adults with diabetes. Link
References:
- American Diabetes Association, 9. Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes—2023. Diabetes Care 1 January 2023; 46 (Supplement_1): S140–S157. https://doi.org/10.2337/dc23-S009
- American Diabetes Association, 13. Older Adults: Standards of Care in Diabetes—2023. Diabetes Care 1 January 2023; 46 (Supplement_1): S216–S229. https://doi.org/10.2337/dc23-S013
- Mounjaro (tirzepatide) injection package insert. Indianapolis, IN:Eli Lilly and Company.; 2022 May




